SPH Student Explores Amish and Plain Anabaptist Culture to Facilitate Partnerships with Local Health Departments
By Erin Frick
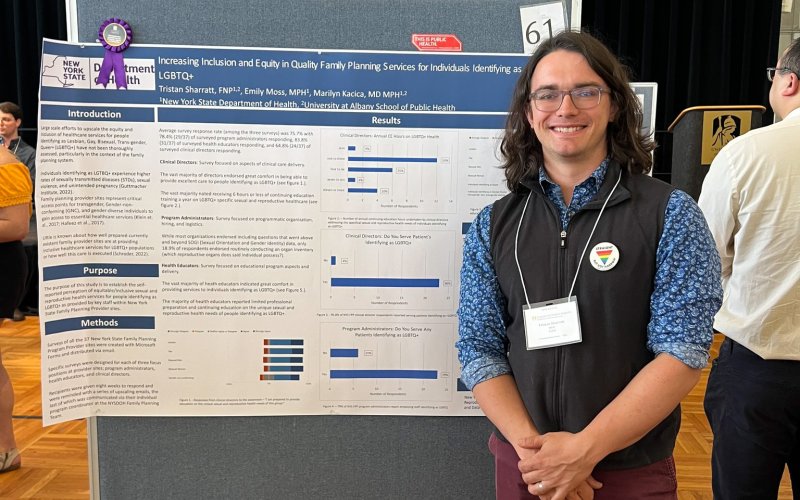
ALBANY, N.Y. (Aug. 29, 2024) — University at Albany’s Tristan Sharratt, a master of public health (MPH) student at the School of Public Health (SPH), harbored a longstanding interest in the field before joining the NYS Fellowship in Applied Public Health (FAPH) program in 2022.
A registered nurse and family nurse practitioner, the Otsego County native has practiced as a nurse in a county jail and a rural public school district.
“My clinical training gave me the practical capability to diagnose, prescribe and function as a healthcare provider, but I always wanted to do more at a larger community level,” said Sharratt. “So, I knew I was headed towards public health in some fashion. I just wasn't quite sure what it was. I learned about the Fellowship in Applied Public Health program while completing the rural family practice portion of my FNP residency. Working closely with the program’s director, we were able to craft a tailored program to support my interests and professional goals.”
The Fellowship in Applied Public Health program is jointly sponsored by UAlbany and the New York State Department of Health. This two-year public health training program is for physicians, veterinarians and other advanced licensed health care professionals with an interest in pursuing leadership roles in state and local health departments. Over the course of the program, fellows earn an MPH with a concentration in population medicine from UAlbany, alongside practical experiences at the New York State Department of Health and a local county health department. Tuition is fully covered, and fellows earn a salary for their work during the program.
As a current FAPH fellow, Sharratt’s role at the NYS Department of Health includes working on the Title V Maternal and Child Health Grant, which aims to improve birth outcomes and promote healthy children and families, and the Early Intervention Program for infants and toddlers with disabilities.
Exploring Health in Rural Communities
Sharratt developed a special interest in rural, community-centric clinical care by observing the model of practice undertaken at the health clinic in his hometown of Cherry Valley in Otsego County.
“The clinical practice was run by two nurse practitioners, one of which became a very good friend of mine,” said Sharratt. “It's one of the few clinics in our region that does home visits and takes social determinants of health into account in planning and delivering services. That was where I learned about how to do clinical care and where my thoughts about how to care for a population grew.”
The Otsego County Department of Health, where Sharratt worked as part of the FAPH program, maintains a unique relationship with local Amish and Plain Anabaptist communities. When, in the early 2000s, an Amish child presented with pertussis (whooping cough), the child’s community reached out to the health department to request vaccines. The county quickly vaccinated all the adults and thus established the program of routine vaccinations that exists today.
“The Otsego health department now wants to expand vaccine efforts into the three other Amish communities in the county, especially in areas where vaccination rates are low,” said Sharratt. “Measles and chickenpox, which are on the rise, are top concerns. As a Fellow, I was tasked with designing a campaign to promote vaccines in these communities. However, if we want to share information on important health tools and encourage uptake, we first need to learn more about these communities and understand how their beliefs and traditions might shape perceptions of these different health tools.”
Community-Informed Care
Since November 2023, Sharratt has continued to dive deep into sociodemographic research focusing on the belief systems and geographic origins of Amish communities in central New York State.
“In my earliest research, I came to realize that there isn’t much advice for clinical professionals and public health professionals looking to interact with these communities to discuss health issues like vaccines and well contamination,” said Sharratt. “It’s also clear that non-Amish people approach Amish communities with broad, often incorrect assumptions about who they are, what they believe and how they behave.”
To learn more, Sharratt has established contact with Amish studies scholars throughout the country. He is currently working with The Places Institute, a demography institute at SUNY Oneonta, on a population study focused on groups of people in central New York that are generally categorized as “white of German ancestry” but represent a wide diversity of groups (including over a dozen distinct Amish, Plain Anabaptist, Mennonite and Hasidic Jewish communities) all with different geographic origins and belief systems that would affect health and healthcare.
Sharratt is also collaborating with scholars affiliated with the Amish and Plain Anabaptist Studies Association who have connected with traditional healers in these communities to learn about traditional practices and explore ways that these methods could enhance, or be applied alongside, western medicine — to the benefit of people within and beyond these communities. Burn remedies are a current focus.
“Many Amish and Plan Anabaptist communities are not as ‘anti-Western medicine’ as many people perceive them to be,” said Sharratt. “However, in this post-covid era, many of these communities have received more vaccine misinformation and disinformation, and less good information on the safety and efficacy of vaccines. As a result, there is a building of resistance to vaccines and other modern public health and clinical health tools. We are hoping to counter that.
“My work now is focusing on how happy accidents – like the connection in Otsego County, where the Amish community reached out to the health department – come to pass. How do we replicate that, even though the social and political context is drastically different now, compared to when that vaccine program initially began over two decades ago?
“As a health department, we need to provide consistent, easy to understand, relatable information that clearly communicates how certain health interventions can be beneficial. This is a challenge that requires a deep understanding of the communities and their traditional practices. My work is about understanding the Amish and building relationships with them such that we have a common understanding about how each other thinks and functions so that we can reach a common ground on some of these critical public health interventions that could protect entire communities in the future.”